Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), named after the 2019 novel coronavirus (COVID-19), is a viral disease that was discovered in late 2019 in Wuhan City, Hubei Province of China, and has spread rapidly around the world(Reference Khanna, Cicinelli and Gilbert1). As of 4 December 2021, the incidence of coronavirus in the world is 265 million people, and the mortality rate is 5·24 million people. in Iran, almost 130 000 people have lost their lives due to coronavirus(Reference Miller2). The disease has imposed a heavy economic burden on the health system(Reference McArthur, Sakthivel and Ataide3,Reference Jin, Wang and Li4) and can cause lifelong damage to the body’s organs(Reference Yelin, Wirtheim and Vetter5). The severity of clinical manifestations and mortality rate of COVID-19 varies from person to person(Reference Baj, Karakuła-Juchnowicz and Teresiński6) and is strongly dependent on the individuals’ immune system(Reference Paces, Strizova and Smrz7). Nutrition and dietary components as modifiable factors can play a bilateral role in strengthening or weakening the immune system(Reference Venkatraman and Pendergast8–Reference Darand, Hassanizadeh and Marzban10). B vitamins (B1, B2, B3, B4, B5, B6, B7, B9 and B12) are a group of water-soluble vitamins that are not synthesised in the human body. So, they must be consumed regularly in the diet. Many body functions, including energy production, methylation, synthesis, DNA repair and enzyme functions, depend on B vitamins’ functions(Reference Herrmann and Obeid11,Reference LeBlanc and de Giori12) . The deficiency of B vitamins suppresses immune functions in multiple ways and increases the susceptibility to infection(Reference Maggini, Pierre and Calder13,Reference Shakoor, Feehan and Mikkelsen14) . Given the anti-inflammatory, antioxidant and immune enhancement effects of B vitamins, it is hypothesised that an adequate intake of rich sources of vitamin B can reduce the risk of COVID-19(Reference Shakoor, Feehan and Mikkelsen14,Reference Manzanares and Hardy15) . Few studies have been conducted on the association between B vitamins and inactivation of the coronavirus(Reference Keil, Ragan and Yonemura16) and B vitamins and reduction of symptoms and damage caused by COVID-19(Reference Desbarats17–Reference Tan, Ho and Kalimuddin20). For example, the results of a review study demonstrated that treatment with cobalamin could improve COVID-19 damage. Another study reported that riboflavin and UV light decreased the titre of SARS-CoV-2 in both plasma and platelet products to below the limit of detection in tissue culture(Reference Keil, Ragan and Yonemura16). In another study, serum levels of vitamin B12 were associated with the clinical outcomes of COVID-19(Reference Shakeri, Azimian and Ghasemzadeh-Moghaddam21). An observational study in Spain also found that 42·5 % of patients with COVID-19 had low levels of vitamin B6 (Reference Tomasa-Irriguible, Bielsa-Berrocal and Bordejé-Laguna22). This study can provide an association between dietary B vitamins and COVID-19 which may lead to other studies to be conducted in the future. Therefore, the purpose of the present study was to investigate the association between B vitamins and the COVID-19 incident.
Materials & methods
Study population
This study was conducted on the recruitment phase data of the Yazd Health Study (YAHS) and Taghzieh Mardom-e-Yazd (TAMIZ) that were conducted on a large sample of Iranians (www.yahs-ziba.com). YaHS is a population-based prospective cohort study designed to assess the changing incidence of a variety of chronic diseases and their associated risk factors among Iranian adults (aged 20–69 years) in Yazd, Iran. TAMIZ is a population-based prospective cohort study designed to assess the changing dietary habits and intake among Iranian adults (aged 20–69 years) in Yazd, Iran. For the present study, the data from both studies (YaHS and TAMIZ) were merged. Dietary information was extracted from the TAMIZ study, and other data were extracted from the YaHS study. Our survey initially included 10 208 adults, but 1019 were excluded due to unusual dietary intake (more than 6500 kcal and less than 600 kcal), taking dietary supplements containing B vitamins and having any type of cancer. Therefore, we ended up with 9189 adults for the final analysis. Please see the participants’ selection algorithm (https://academic.oup.com/ije/article/47/3/697/4658812). The participants were selected from September 2014 to March 2016 based on the two-stage cluster sampling method according to the WHO STEP guidelines. First, 200 clusters were randomly selected based on the postal code of the city of residence. Second, the study was presented to them by interviewers, and they organised a meeting time at their domiciles. Finally, interviewers met fifty participants defined for each cluster (twenty-five men and twenty-five women) to interview based on the study protocol. There are five persons in each 10-year age group (20–29, 30–39, 40–49, 50–59 and 60–69 years). Moreover, due to the cohort nature of the YaHS study, the information is updated every 5 years and the incidence of various diseases is measured. According to the worldwide COVID-19 epidemic, the incidence of COVID-19 among participants was measured.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the ethics committee of Shahid Sadoughi University of Medical Sciences (Ethical approval code: IR.NIMAD.REC.1395·001, Date: 8 July 2014).
First, all participants signed informed written consent. Data on participants’ general characteristics, history of chronic disease, physical activity, smoking history, anthropometric measurements and dietary assessment were collected using validated questionnaires. In order to evaluate the validity and reliability of the questionnaires, a pilot study was conducted on fifty participants before the start of the main study, and the results were reported and published by experts in each section. The reliability of the questionnaires was also confirmed by Cronbach’s α of 0·89. More details of YaHS have been published elsewhere(Reference Mirzaei, Salehi-Abargouei and Mirzaei23). In addition to the previous questionnaires, a specific COVID-19 questionnaire was completed over the phone for all participants who were diagnosed with COVID-19 from February 2020 to February 2021, according to the Yazd Central Health database. In this questionnaire, they were asked whether or not they had undergone a diagnostic test for COVID-19. PCR tests were collected from participants. But our team conducted a PCR test for those without a PCR test or other diagnostic tests.
COVID-19 incidence measurement
The basis of the diagnosis of COVID-19 was PCR tests.(Reference Tahamtan and Ardebili24). The results of the PCR test were either reported by the participants themselves or the participants came back to the study team if they had symptoms or a COVID-19 suspicion, in which case the PCR test was performed by our research team. Also, serologic assays were used to estimate IgM and IgG antibodies in symptomatic or asymptomatic COVID subjects recovered from the disease. Serologic assays involving IgM and IgG antibodies to detect antibodies against SARS-CoV-2 were used as these antibodies can be detected from the second week of the start of COVID-19 symptoms, where IgM can be detected after the fourth day of infection and IgG has been found after the eighth day of disease onset. Serologic assays provide quick diagnostics by avoiding PCR false-positive or false-negative results. Additionally, these assays provide antibody patterns for the estimation of the strength and duration of humoral immunity(Reference Nakano, Kurano and Morita25).
Dietary assessment
Dietary intake was assessed in 2014–2016 using a 178-item semi-quantitative FFQ consisting of 551 questions about dietary intake over the past year(Reference Mirzaei, Salehi-Abargouei and Mirzaei23). In this FFQ, the intakes of all food groups, such as grains, fruits and vegetables, dairy products, legumes, sweets, and oils, were examined. The FFQ used in TAMIZ was a modified version of a previously validated 168-item FFQ applied to the Tehran Lipid and Glucose Study (TLGS). Ten items commonly consumed by Yazdi adults were added to the original 168-item FFQ, resulting in a 178-item FFQ. Furthermore, the 168-item FFQ used in TLGS was originally designed to be open-ended; however, in TAMIZ, we changed the questionnaire to a multiple-choice one. Also, in order to obtain accurate estimates, we rendered the portion size of food as a unit using a photo book for all participants. Two types of questions were asked of the participants about each food item: (1) the frequency of food consumption (number of times per month, week or day the food was consumed) in the previous year, and (2) the amount of the food that was usually consumed every time (portion size based on the standard serving sizes commonly consumed by Iranians). All reported intakes were converted to g/d by using household measures of consumed foods. Then we used Nutritionist IV software to calculate nutrient intakes(Reference Bodner-Montville, Ahuja and Ingwersen26). The total B vitamins intake for each person was obtained by summing the content of B vitamins of all food items eaten. Recently, a subgroup of this cohort study’s participants was asked if their eating habits had changed over the past few years, and the answer was no. In addition, because the participants live in a city whose people are conservative(Reference Abbasi-Shavazi and McDonald27), their dietary patterns have not changed in the last 5 years, and their answers can be generalised to all participants. Also, considering the cohort nature of the data study and the effect of dietary patterns on the immune system over time, the association is justifiable because the immune system has a direct effect on the incidence of the disease. The questionnaire was designed by a trained reviewer.
Anthropometric measurements
Participants’ weight was measured using a portable digital scale and the body analyzer (Omron Inc.), with an accuracy of 0·1 kg, with a minimum of clothing and without shoes. Height was measured in a standing position without shoes, with their heads in the Frankfurt position and their shoulder blades touching the straight wall to which the tape was attached. Also, BMI was calculated as weight (kg) divided by height squared (m).
Physical activity assessment
The level of daily PA was assessed using the short form of the International Physical Activity Questionnaire (IPAQ). PA is classified as low, medium and high according to the guidelines of the IPAQ short form(28). The Persian translation validation of IPAQ was previously confirmed by Moghaddam et al.(Reference Moghaddam, Aghdam and Jafarabadi29).
Statistical analysis
Study participants were categorised into quartiles based on their B vitamins intake in three models. The first category (the lowest intake) was considered as a reference. The second quartile was considered as the low intake, the third quartile as the moderate intake and the last quartile as the highest intake. Frequency and percentage were used to describe the qualitative variables. Multivariable logistic regression analysis was performed in different models to find the association between B vitamins intake and COVID-19. In model 1, we adjusted only age and total energy intake. In model 2, smoking status, physical activity, marital status, educational level, chronic disease, sex, physical activity, job status, house status (homeowner or tenant) and ethnicity (from Yazd or not from Yazd) were additionally adjusted. Final adjustments were made for BMI. Logistic regression results were reported as the OR and 95 % CI. All analyses were performed using the SPSS software (version 22; SPSS Inc). P-values < 0·05 were considered statistically significant.
Results
Characteristics of participants
We studied 9189 Iranian adults (48·4 % were men). Sixty-one per cent of participants were under 50 years old, 85 % were married, 15·5 % graduated from university, 86·9 % had never smoked, and 64·5 % were obese or overweight. In addition, 832 out of 9189 participants were infected with the coronavirus (9·1 %) (Table 1).
Table 1. The distribution of the Yazd Health Study (YaHS) participants according to general characteristics
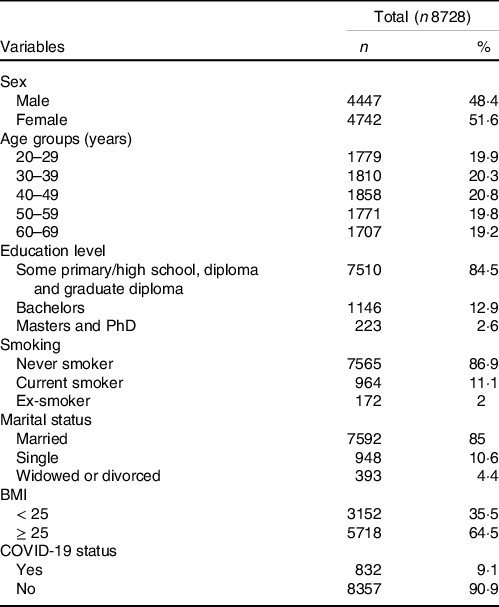
BMI is calculated as weight in kilograms divided by height in metres squared.
Dietary B vitamins intake and coronavirus
Multivariable-adjusted OR and 95 % CI for COVID-19 and B vitamins intake are shown in Table 2. Higher intake of vitamin B5 (quartile 4) compared with the lowest intake (quartile 1) had a protective effect on COVID-19 after adjusting for model 3 (OR: 0. 53, CI 0·28, 0·99, P-trend = 0·02).
Table 2. Multivariable adjusted OR and 95% CI for COVID-19 and B vitamin intake across quartiles of consumption in a sample of Iranian adults
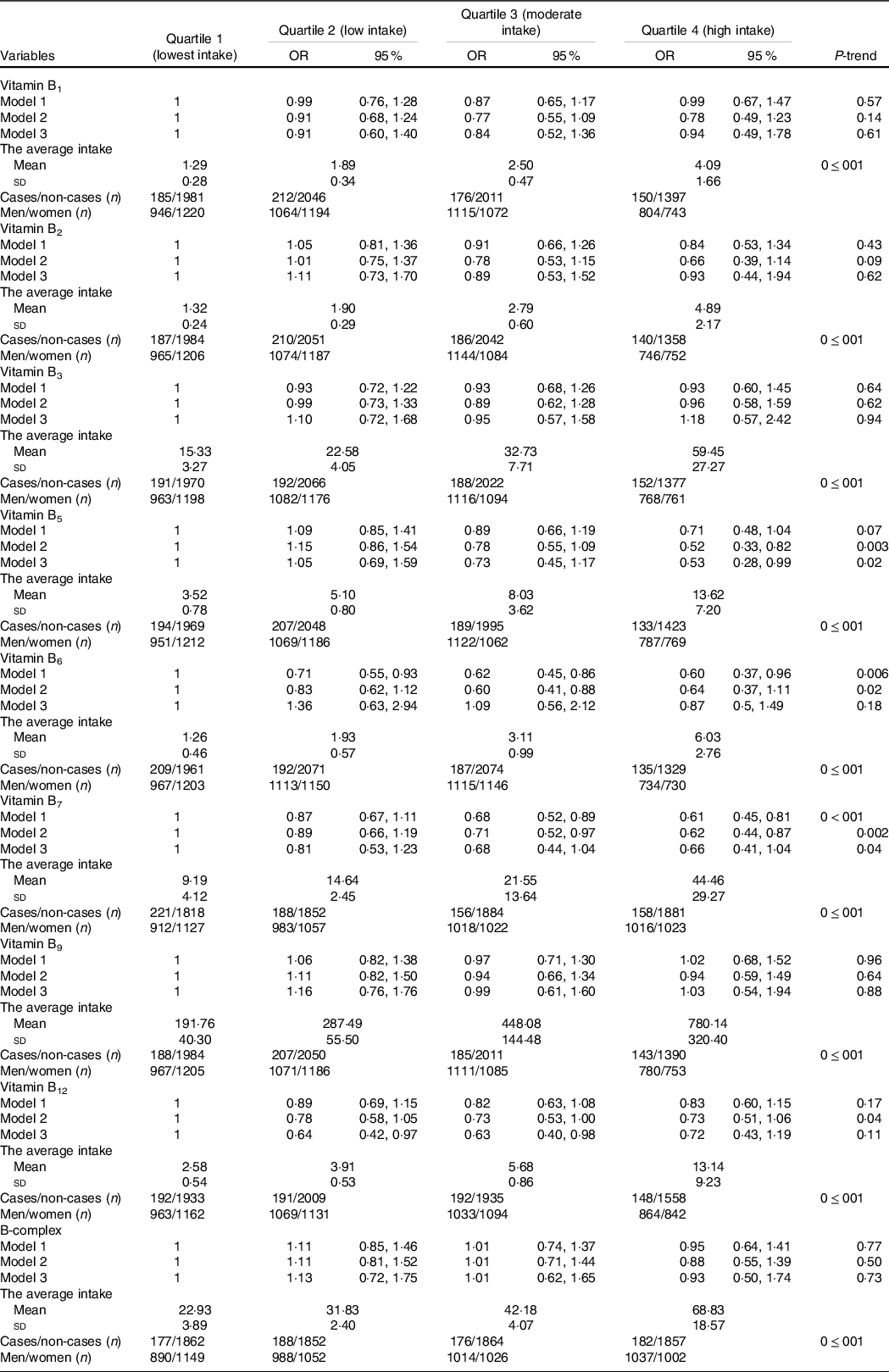
Values are reported as OR and 95% CI and mean (sd).
All average intakes were reported in mg except for B7, B9, and B12 which were reported in mcg.
Model 1: Adjusted for age and energy intake.
Model 2: model 1+ further adjustment for smoking status, physical activity, marital status, educational levels, chronic disease, sex, job status, house status (homeowner or tenant), ethnicity (from Yazd or not from Yazd).
Model 3: model 2+ further adjustment for BMI.
The Recommended Dietary Allowance (RDA) of B1, B2, B3, B5, B6, B9, and B12 for men ages 19 and older is 1·2 mg, 1·3 mg, 16 mg, 5 mg, 1·3 mg, 400 mcg, and 2·4 mcg daily and for women in the same age range is 1·1 mg, 1·1 mg, 14 mg, 5 mg, 1·3 mg, 400 mcg, and 2·4 mcg daily respectively. An RDA does not exist for B7. Instead, the AI (Adequate Intake) level, for B7 for men and women 19 years and older is 30 mcg daily.
The highest intake of B6 and B7 (quartile 4) compared with the lowest intake (quartile 1) was associated with a lower odd of COVID-19 after adjusting for model 1 (OR B6:0·60, CI 0·37, 0·96, P-trend = 0·006) and model 2, respectively (OR B7:0·62, CI 0·44, 0·87, P-trend = 0·002). This significant association disappeared after further adjusting for BMI.
Moderate intake of vitamin B12 (quartile 3) compared with the lowest intake (quartile 1) (OR: 0·63, 95 % CI 0·40, 0·98, P-trend = 0·11) could reduce the odds of COVID-19 after adjusting for model 3. Our findings indicated no significant relationship between dietary intake of vitamin B1, B2, B3, B9 and B-complex and COVID-19.
In addition, there is a significant difference in the intake of B vitamins based on quartiles of consumption (P < 0·05). The intakes of our population in the fourth quartile compared with the RDA values for all B vitamins were multi-folded (Table 2).
Subgroup analysis based on BMI
An analysis stratified by BMI indicated that the highest intake of vitamin B5 (quartile 4) compared with the lowest intake (quartile 1) significantly reduced the odds of COVID-19 in both groups after full controlling for confounders (OR BMI < 25:0·45, CI 0·27, 0·77, P-trend = 0·003) and (ORBMI ≥ 25:0·02, CI 0·001, 0·62, P-trend = 0·01).
After controlling for confounders, the highest consumption of B7 (quartile 4) (OR: 0·56, CI 0·38, 0·84, P-trend = 0·001) and B12 (OR: 0·62, CI 0·41, 0·95, P-trend = 0·01) compared with the lowest consumption (quartile 1) could significantly decrease the odds of COVID-19 only in individuals with BMI less than 25. However, the highest intake of vitamin B6 (quartile 4) compared wih the lowest intake (quartile 1) (OR 0·01, 95 % CI 0·001, 0·74, P-trend = 0·02) could significantly decrease the odds of COVID-19 among those with a BMI greater than 25 after controlling for all possible confounders (Table 3).
Table 3. Multivariable adjusted OR and 95% CI for COVID-19 based on B vitamins intake quartile stratifying by BMI
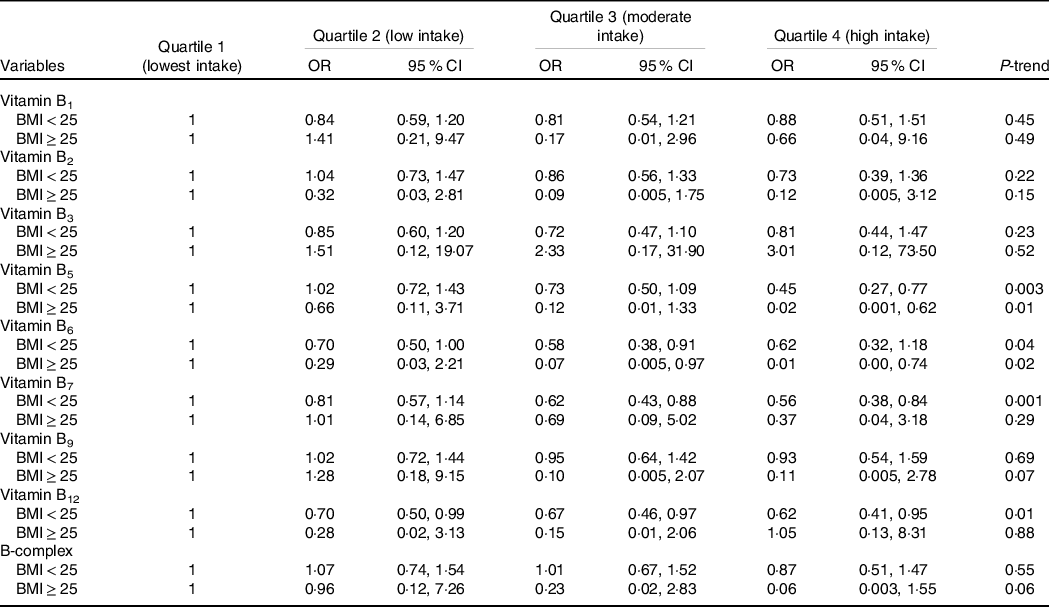
Values are reported as OR and 95% CI.
All values are adjusted for age, sex, energy intake, smoking status, physical activity, marital status, educational levels, chronic disease, job status, house status (homeowner or tenant) and ethnicity (from Yazd or not from Yazd).
Subgroup analysis based on chronic disease status
Stratified analysis based on chronic disease status (participants with at least one chronic disease, including high blood pressure, diabetes, CVD and dyslipidemia) indicated that the highest dietary intake of B9 (quartile 4) (OR: 0·05, CI 0·006, 0·53, P-trend = 0·04) and B-complex compared with the lowest intake (quartile 1) (OR: 0·01, CI 0·001, 0·17, P-trend = 0·01) could significantly decrease the odds of COVID-19 in participants who have at least one chronic disease. In addition, moderate consumption of B7 (quartile 3) (OR: 0·60, CI 0·37, 99, P-trend = 0·02) and B12 (OR: 0·58, CI 0·35, 0·98, P-trend = 0·14) compared with the lowest consumption (quartile 1) could decrease the odds of COVID-19 in participants who have no chronic disease after adjustments for all possible confounders (Table 4).
Table 4. Multivariable adjusted OR and 95% CI for COVID-19 based on B vitamins intake quartile stratifying by chronic disease status
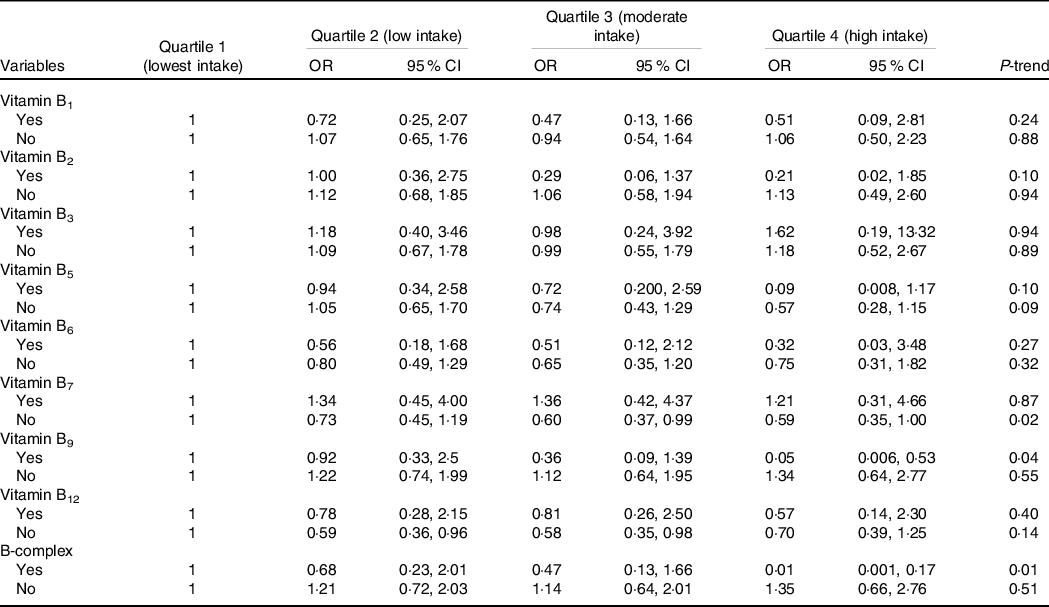
Values are reported as OR and 95% CI.
All values are adjusted for age, sex, energy intake, smoking status, physical activity, marital status, educational levels, job status, house status (homeowner or tenant), ethnicity (from Yazd or not from Yazd) and BMI.
Subgroup analysis based on sex
Stratified analysis based on sex indicated that the highest intake of vitamin B6 (quartile 4) in women compared with the lowest intake (quartile 1) could reduce the odds of COVID-19 after adjustments for all possible confounders in model 3 (OR: 0·07, CI 0·006, 0·84, P-trend = 0·01), while the moderate intake of vitamin B6 (quartile 3) (OR: 0·66, CI 0·44, 0·97, P-trend = 0·08) in men compared with the lowest intake (quartile 1) was able to reduce the odds of COVID-19 after adjustments for all possible confounders. In addition, men with the highest intake (quartile 4) of vitamin B5 (OR: 0·55, CI 0·34, 0·88, P-trend = 0·009) and B7 (OR: 0·64, CI 0·45, 0·90, P-trend = 0·003) have shown the reduced odds of COVID-19 compared with those with the lowest intake (quartile 1) after full adjustments in model 3.
Discussion
In this relatively large population-based study of Iranian participants, we observed a statistically significant inverse association between dietary intake of B vitamin groups and the risk of COVID-19. The decreased odds of COVID-19 were limited to vitamins B5, B6, B7 and B12, and no significant odds reduction were observed for dietary intake of vitamins B1, B2, B3, B9 and B-complex.
Previous studies have mainly focused on the effect of dietary supplementation on COVID-19 risk reduction(Reference Khalagi, Gharibzadeh and Khalili30–Reference McPherson, Keunen and Bird34). However, a large app-based community survey of 445 850 subjects in the UK, USA and Sweden reported that specific nutrients or dietary supplements are associated with modest reductions in COVID-19 risk (9–14 %)(Reference Louca, Murray and Klaser35). Our findings are in line with preliminary evidence indicating that optimal nutrition status may reduce the risk of infectious diseases(Reference Calder36–Reference Farhadi and Ovchinnikov39). Furthermore, several documents suggest the protective role of a balanced diet in COVID-19(Reference Jayawardena and Misra40–Reference Lohi and Sawarkar43). The results of a large survey indicated that high-diet quality was associated with lower risk and severity of COVID-19(Reference Merino, Joshi and Nguyen44). Another observational study in China investigated the relationship between nutritional status and clinical outcomes in patients with SARS-COV-2 infection. They found that patients with higher nutritional risk had worse outcomes, including a higher risk of mortality and more extended hospital stay(Reference Zhao, Li and Ge45). Interestingly, diet is also proposed as a potentially responsible factor for differences in COVID-19 death rates between and within countries(Reference Bousquet, Anto and Iaccarino46). Therefore, based on the available evidence, not only may an appropriate diet containing an optimal amount of micronutrients and macronutrients play a preventive role against COVID-19 but also it can attenuate the clinical consequences in the affected person. Among the B vitamins evaluated in this study, dietary intake of vitamin B5 showed the highest protective association with COVID-19. Dietary intake of vitamin B5 was associated with about a 50 % reduction in the odds of COVID-19 when comparing the highest to the lowest quartile of intake. The protective effect of vitamin B5 may partially be explained by its involvement in immune response as well as its anti-inflammatory properties(Reference Jung, Kim and Choi47–Reference Gheita, Gheita and Kenawy49). Vitamin B5 boosts macrophage maturation, increases macrophage phagocytosis, and promotes Th1 and Th17 cell differentiation(Reference He, Hu and Du50).
The highest intake of B6 and B7 was also associated with a lower odd of COVID-19. However, this significant association disappeared after further adjustment for BMI. Unlike B5, B6 and B7, whose highest intake was associated with the lowest risk of COVID-19, only moderate intake of B12 contributed to a significant reduction in the odds of COVID-19.
We also found evidence of a modifying effect of BMI, sex and chronic disease status on the association between B vitamins intake and the risk of COVID-19. A high dietary intake of vitamins B6 and B5, compared with the lowest intake, reduced the odds of COVID-19 in subjects with BMI ≥ 25. However, a high intake of vitamins B5, B7 and B12 compared with the lowest intake reduced the odds of COVID-19 among individuals with a BMI of less than 25. Therefore, it seems that the relationship between dietary intake of B vitamins and the risk of COVID-19 is affected by BMI. In addition, a high dietary intake of vitamins B5 and B7 compared with the lowest intake could reduce the odds of COVID-19 only in men. The significance of these findings is that men and subjects with BMI ≥ 25 are at higher risk for COVID-19 and its mortality(Reference Gheita, Gheita and Kenawy49,Reference He, Hu and Du50) . The association between folic acid and COVID-19 has been suggested by recent studies(Reference Meisel, Efros and Bleier51,Reference Wiltshire, Peña and MacKenzie52) . A recent study demonstrated that folic acid inhibits the proteolytic protein furin, which promotes coronavirus activation(Reference Meisel, Efros and Bleier51). Although in our main analysis, we did not find a significant relationship between dietary intake of vitamin B9 and B-complex and risk of COVID-19, stratified analysis based on chronic disease status revealed a protective effect on COVID-19 in the highest quartile in participants who have at least one chronic disease. In the present study, the average consumption of folic acid in participants who have at least one chronic disease in comparing those without chronic disease was less. These findings may be attributed to the fact that B vitamins, including vitamin B9, contribute to the healthy balance of the immune system. Additionally, vitamin B9 is involved in the production of nucleic acids, protein synthesis, and involvement in crucial metabolic processes, such as methylation and the serine, glycine, and purine cycles. Inefficient methylation can result in hyperhomocysteinemia, which contributes to the pathogenesis of many diseases(Reference Mikkelsen, Apostolopoulos, Mahmoudi and Rezaei48). Hence, a high intake of B vitamins, especially B9 in the chronic diseases group, may alleviate these conditions.
Interestingly, in the case of B7 and B12, significant inverse associations were observed only across moderate consumption in participants who had no chronic disease. This can indicate that each micronutrient in its optimal amount can have protective effects, and not necessarily the higher the intake, the lower the risk of disease. In addition, a previous study revealed that there is a positive association between vitamin intake and plasma concentrations. However, determinants such as sex, age and energy intake should be considered(Reference Baart, Balvers and de Vries53).
The observed inverse associations between B vitamins intake and COVID-19 risk may be explained by their influence on a variety of biological functions. B vitamins are involved in cell functioning, energy metabolism and proper immune function(Reference Mikkelsen, Apostolopoulos, Mahmoudi and Rezaei48). B vitamins play an important role in the proper activation of both the innate and adaptive immune responses; they suppress the secretion of pro-inflammatory cytokines; they enhance respiratory function; they support endothelial integrity; besides, they can shorten hospital stays(Reference Shakoor, Feehan and Mikkelsen14,Reference Michele, Angel and Valeria54,Reference Mahmoudi and Rezaei55) . Some evidence suggests B vitamins deficiency can significantly impair cell and immune system function and contribute to inflammation resulting from hyperhomocysteinemia(Reference Mikkelsen, Apostolopoulos, Mahmoudi and Rezaei48,Reference Mahmoudi and Rezaei55) .
Notably, the B vitamins have been shown to have an intestinal bacterial source and a food source, suggesting that the normal intestinal microbiome may have always been the primary source of B vitamins(Reference LeBlanc, Milani and De Giori56). However, several factors, including lifestyle changes following lockdown and vitamin D deficiency, change the intestinal microbiome, reducing B vitamin production in the gut(Reference Gominak57,Reference Zuo, Wu and Wen58) . Considering the beneficial effects of B vitamins in reducing COVID-19 risk and the possibility of disruption in intestinal production of B vitamins, dietary intake of these vitamins needs more attention. Therefore, considering enough intake of rich foods of B vitamin within a healthy diet could lead to attenuating the odds of COVID-19
In this study, no association was found between the intake of vitamins B1, B2 and B3 with the odds of COVID-19, neither in the total analysis nor in the subgroup analyses. These results align with the Deschasaux-Tanguy et al. study(Reference Deschasaux-Tanguy, Srour and Bourhis59). These results are unclear but may be explained by the fact that COVID-19 patients may not suffer from these vitamin deficiencies. Our study investigated the association between dietary intake of B vitamins and the risk of COVID-19 in a large sample of Iranian adults. However, several limitations should be considered in this study. First, recall bias may not be exactly excluded because of the retrospective nature of dietary assessment by FFQ. Second, as an observational study, we are unable to show a causal relationship between B vitamins and COVID risk. Third, we could not assess the correlations between B vitamins intake and plasma levels. Fourth, no information on COVID-19 severity was available. In addition, although we considered the most important confounding variables, there would be some residual confounders that we failed to assess
Conclusion
In conclusion, an inverse association between dietary intake of B vitamins and the risk of COVID-19 was observed in the current study. Results from this study could expand previous findings on nutrition implication in COVID-19 risk and highlight the potential protective effects of dietary intake of B vitamins. Our data support the hypothesis that individuals should not only rely on dietary supplements and adherence to a healthy diet consisting of an optimal amount of macronutrients and micronutrients, especially B vitamins, which could be beneficial in preventing COVID-19. Although the protective role of nutrients against COVID-19 seems promising, further research is needed to better understand the different nutrient implications in both prevention and treatment of COVID-19.
Acknowledgements
Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
This article has no funding.
M. H.: supervision, study concept and design analysis of data, review and editing; M. D.: drafting the manuscript; S. H.: analysis of data and statistical analysis; A. M.: data collection; M. M.: revising the manuscript; and F. M. and S. S.: writing the manuscript. The authors declare no conflicts of interest related to this study.







